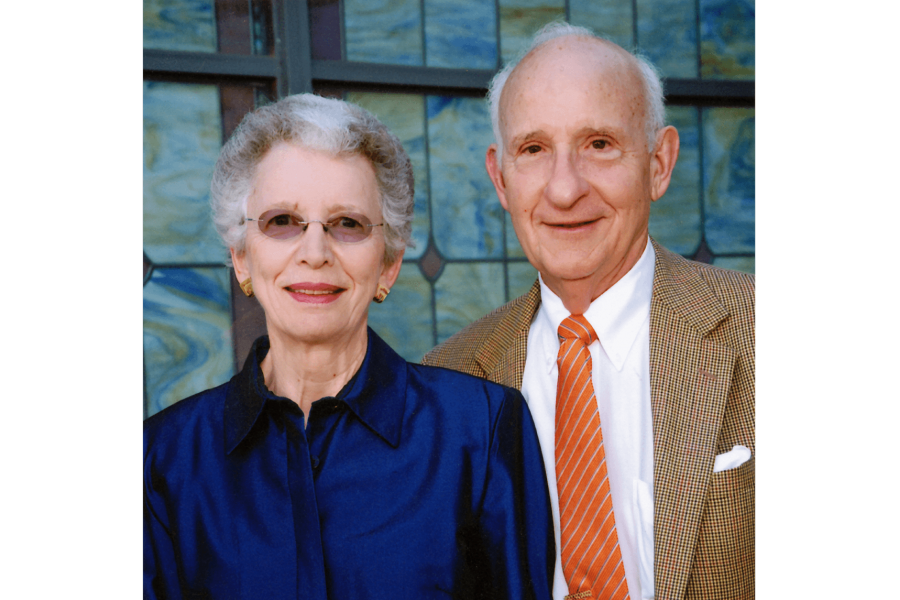
In 2016, Ernest and Evelyn Rady, through the Rady Family Foundation, committed an unprecedented $30 million to support the Faculty of Health Sciences, which is now known as the Rady Faculty of Health Sciences.
Ernest [BComm/58, LLB/62, LLD/15] and his wife Evelyn [BA/60, BSW/61, MSW/67] dedicated the gift to the legacy of his parents, Rose and Max Rady [MD/21]. The latter was a UM-educated physician and namesake of the Max Rady College of Medicine.