 |
 |
|
| Neurovascular compression of the trigeminal nerve root entry zone leads to hyperactivity of the trigeminal nerve nucleus. | Medical therapy aims to reduce hyperactivity of the trigeminal nerve nucleus, thereby reducing attacks of TN pain. |

 |
 |
|
| Neurovascular compression of the trigeminal nerve root entry zone leads to hyperactivity of the trigeminal nerve nucleus. | Medical therapy aims to reduce hyperactivity of the trigeminal nerve nucleus, thereby reducing attacks of TN pain. |

Almost all typical
TN sufferers experience significant pain relief with carbamazepine. The
starting daily dose is low, (one to two pills a day), which is gradually increased
until the pain is completely alleviated or side effects occur. Good relief of
pain may be achieved at low doses, but the usual effective dose ranges from
600 to 1600 mg divided in three or four doses per day. Even higher doses may
be required during severe attacks of pain. Once relief of the pain has been
achieved, the same dose is usually continued for at least two weeks before trying
to reduce to a minimal dosage that provides pain relief. As with all TN medications,
TegretolŽ may gradually be decreased during periods of remission.
Several dose-related side effects are often experienced including drowsiness, mental confusion, dizziness, nystagmus (rapid movements of the eye), ataxia (decreased coordination), diplopia (double vision), nausea, and anorexia (loss of appetite). If side effects are severe, the daily dose of carbamazepine may be decreased for 1 to 3 days, before trying to increase the daily dose again.
There are also rare but serious reactions to carbamazepine
that are not dose related. These include an allergic skin rash that may form
any time after the medication is started. Two to six percent of sufferers who
take carbamazepine develop blood disorders including leukopenia or agranulocytosis
(drop in the number of white blood cells), or aplastic anemia (when the bone
marrow stops producing blood cells) . Other rare complications include liver toxicity, water intoxication (retention of water), hyponatremia (low sodium in the blood), congestive
heart failure, visual hallucinations and disorders of taste or sexual function.
Due to these complications, blood tests are usually conducted before carbamazepine
is started, and repeated intermittently. The administration of carbamazepine
should be discontinued if the white blood cell counts become abnormally low.
A physician should be notified immediately and blood tests conducted if one
experiences a fever, sore throat, stomatitis (painful infection of the mouth),
easy bruising, or petechiae (tiny red spots on the skin).
Oxycarbamazepine
is a new form of Tegretol® that may involve fewer side effects and risks
of toxicity, but must be taken in higher doses to provide adequate pain control.
Trileptal, or oxycarbemazepine, is a form of Tegretol® that is becoming more widely prescribed for a variety of conditions. It has recently been found to be effective for some patients with trigeminal neuralgia. Like Tegretol®, it is an anti-seizure drug, but the side effects are less severe and less frequently experienced.
The dose usually begins at 300 mg twice a day and is gradually increased to achieve pain control. The maximum dose is 2400-3000 mg per day. Common side effects are nausea, vomiting, dizziness, fatigue and tremors. Less frequent symptoms are rash, respiratory infections, double vision, and changes in electrolytes in blood. If you have had an allergic reaction to Tegretol® (carbemazepine), then you should not try Trileptal. As with other anti-seizure medications, increasing and decreasing the dose should be gradual.
 Phenytoin
relieves tic pain in over half of TN sufferers
at doses of 300 to 500 mg, divided into three doses per day. Phenytoin may also
be administered intravenously to treat severe exacerbations of TN. The maximum
dose depends upon the severity of the side effects that are experienced with
the drug. These dose-dependant side effects include nystagmus (rapid movements
of the eye), ataxia (decreased coordination), dysarthria (speech difficulty),
ophthalmoplegia (paralysis of eye movements) as well as drowsiness and mental
confusion. Other effects of the medication may include gingival hyperplasia
(enlargement of the gums in the mouth) and hypertrichosis (excessive hair growth).
Rare but serious complications may occur, including allergic skin rashes, liver
damage and blood disorders.
Phenytoin
relieves tic pain in over half of TN sufferers
at doses of 300 to 500 mg, divided into three doses per day. Phenytoin may also
be administered intravenously to treat severe exacerbations of TN. The maximum
dose depends upon the severity of the side effects that are experienced with
the drug. These dose-dependant side effects include nystagmus (rapid movements
of the eye), ataxia (decreased coordination), dysarthria (speech difficulty),
ophthalmoplegia (paralysis of eye movements) as well as drowsiness and mental
confusion. Other effects of the medication may include gingival hyperplasia
(enlargement of the gums in the mouth) and hypertrichosis (excessive hair growth).
Rare but serious complications may occur, including allergic skin rashes, liver
damage and blood disorders.
 Baclophen
is not as effective as carbamazepine or phenytoin for TN, but may be used in
combination with these medications. The starting dose of baclophen is usually
5 mg two or three times a day, and may be gradually increased. The usual dosage
taken for complete pain relief is between 50 and 60 mg per day. Baclophen has
a short duration of function so sufferers with severe TN may need to take doses
every 3 to 4 hours.
Baclophen
is not as effective as carbamazepine or phenytoin for TN, but may be used in
combination with these medications. The starting dose of baclophen is usually
5 mg two or three times a day, and may be gradually increased. The usual dosage
taken for complete pain relief is between 50 and 60 mg per day. Baclophen has
a short duration of function so sufferers with severe TN may need to take doses
every 3 to 4 hours.
The most common side effects associated with baclophen include drowsiness, dizziness, nausea and leg weakness. The incidence of these side effects is reduced by starting with a low dose of baclophen that is gradually increased. However, approximately one tenth of sufferers cannot tolerate baclophen. A rare complication is a confusional state that appears shortly after baclophen is started, but this resolves quickly when therapy is stopped. Baclophen should not be discontinued abruptly after prolonged use because hallucinations or seizures may occur. If these withdrawal symptoms do occur, the previous dose of baclophen is usually re-instituted and then gradually reduced.
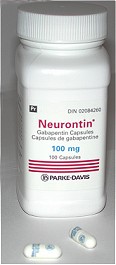 Gabapentin
is an anti-epileptic drug that is structurally related to the neurotransmitter
GABA. This drug is almost as effective as carbamazepine
but involves fewer side effects. The
starting dose is usually 300mg three times a day and this is increased to a
maximal dose. The most common adverse reactions include somnolence (sleepiness),
ataxia (decreased coordination), fatigue, and nystagmus (rapid movements of
the eye). There is no known interaction with TegretolŽ
or DilantinŽ, permitting usage of these drugs in combination
with NeurontinŽ. As with all of these drugs, rapid discontinuation should be
avoided as severe withdrawal reactions may occur.
Gabapentin
is an anti-epileptic drug that is structurally related to the neurotransmitter
GABA. This drug is almost as effective as carbamazepine
but involves fewer side effects. The
starting dose is usually 300mg three times a day and this is increased to a
maximal dose. The most common adverse reactions include somnolence (sleepiness),
ataxia (decreased coordination), fatigue, and nystagmus (rapid movements of
the eye). There is no known interaction with TegretolŽ
or DilantinŽ, permitting usage of these drugs in combination
with NeurontinŽ. As with all of these drugs, rapid discontinuation should be
avoided as severe withdrawal reactions may occur.
Next Section >>
<< Return to Table of Contents
Click
here to return to the
Trigeminal Neuralgia
Web-Site at the Centre for
Cranial Nerve Disorders
A.
M. Kaufmann & M. Patel
Centre for Cranial Nerve Disorders
Winnipeg, Manitoba, Canada
© 2001