Our story
Watch a brief video to learn more about our department and what we offer.
What we offer
The Department of Emergency Medicine trains physicians across all levels to a high degree of excellence. Our education programs reach students the importance of patient centered care, readying them to provide tertiary medicine in an effective and efficient way. We are proud to offer education at the undergraduate and postgraduate level, training the province's next generation of emergency medicine physicians.
Critical care
Critical care focuses on caring for patients with life-threatening conditions who require complex monitoring, organ support, and intensive interventions. In Emergency Medicine, critical care overlaps when patients transition from resuscitation in the ED to the ICU and includes research and quality improvement of that critical phase.
Staff complement
We have four physicians who work as emergency medicine-based intensivists in Manitoba:
- Dr. Eric Flynn
- Dr. Carmen Hrymak
- Dr. Murdoch Leeies
- Dr. Shelly Zubert
Equity, diversity and inclusion (EDI)
EDI focuses on promoting fair, inclusive, and culturally responsive practices in emergency medicine. This encompasses research into health disparities, curriculum development, policy advocacy, and interventions to reduce bias and structural inequities in care delivery.
The Disrupting Racism in Emergency Medicine (DRiEM) research program is one way we are working to improve Manitoba’s emergency departments by understanding and then designing evidence-based strategies to mitigate racism in emergency medicine.
Staff complement
We are also proud to support an interdisciplinary Equity, Diversity and Inclusion Committee led by:
- Dr. Carmen Hrymak
- Dr. Murdoch Leeies
The committee works to identify gaps in knowledge and service, followed by recommendations for best practices, lecture series, and educational modules to enhance health equity, diversity, and inclusion in emergency medicine.
Geriatric medicine
Geriatric medicine centers on the unique needs of older adults, recognizing that aging populations often present with complex comorbidities, atypical symptoms and increased vulnerability to adverse outcomes. In emergency care, this involves tailored assessment, safe transitions and research to reduce repeat visits and hospitalizations.
Staff complement
- Dr. Alecs Chochinov
- Dr. Malcolm Doupe
Both physicians have an international program of research exploring the ways in which acute health care facilities, allied services and community-based care options can be aligned more effectively to help older adults live successfully in the community.
Medical education
Medical education covers the theory and practice of teaching, assessment and curriculum design in emergency medicine. This includes training learners (students, residents, faculty), educational research, mentorship, and innovation in pedagogical methods (e.g., flipped classrooms, competency-based approaches).
Staff complement
- Dr. Tamara McColl serves as the director of education, scholarship and faculty development
- Dr. Zoe Oliver serves as director of the medical education block provided for FRCPC EM residents
Patient and community engagement
Patient and community engagement highlights the partnership between emergency medicine and the communities it serves. This includes involving patients and families in shaping care, collaborating with community organizations, and advancing research, education, and advocacy that reflect patient voices and community needs.
The CEDVIP project provides a 24/7 response to offer support to youth (ages 14–29) who have presented with an injury caused by violence. Youth are offered trauma-informed, flexible follow-up support in the community to assist with reducing their risk and supporting stability to prevent repeat injury.
- The CEDVIP lead is Dr. Zoe Oliver.
The EPIC program, operated by the Winnipeg Fire Paramedic Service (WFPS) and staffed by paramedics, provides early health assessments and intervention planning to Winnipeg patients who are identified as top users of Emergency Medical Services (EMS) and Emergency Department services and who are referred to the program.
- The EPIC lead is Dr. Erin Weldon.
Pediatric emergency medicine (PEM)
PEM specializes in the emergency care of infants, children, and adolescents. It involves understanding age-specific disease patterns, dosing, communication, and procedural skills tailored to younger patients, along with research and collaboration across pediatric centers.
Point of care ultrasound (POCUS)
POCUS emphasizes the use of bedside ultrasound by emergency physicians to rapidly assess, diagnose, and guide procedures in real time. POCUS enhances decision-making in critical situations such as trauma, shock, cardiac arrest, and procedural safety, while also advancing research and education in emerging ultrasound applications.
Curriculum
From the implementation of a formal postgraduate ultrasound curriculum in 2011, training in point-of-care ultrasound (POCUS) continues to be a mandatory skill required for Royal College certification, as well as a critical skill for emergency physicians to improve patient care. The ultrasound curriculum has been designed to include two tracks: core and advanced.
Staff complement
- Dr. Tomislav Jelic serves as the ultrasound director
- Dr. Chitbanu Singh serves as the AFC Acute Care POCUS Fellowship director
- Dr. Joanna Maclean serves as the FRCPC assistant director of ultrasound
- Dr. Caroline Kowal serves as the CCFP assistant director of ultrasound
Pre-hospital
Pre-hospital Medicine covers emergency care delivered before arrival at the hospital (e.g., by paramedics, air medical services). Topics include protocols for out-of-hospital care, early interventions, system design, and integrating prehospital and in-hospital workflows to optimize outcomes. More recently, our physicians have staffed VECTRS (Virtual Emergency Care and Transfer Resource Service).
Staff complement
- Dr. Rob Grierson serves as the chief medical officer of Emergency Response Services
- Dr. John Sokal serves as the medical director of VECTRS
- Dr. Erin Weldon serves overseeing EMS rotations
- Dr. Doug Martin serves as the medical director of STARS
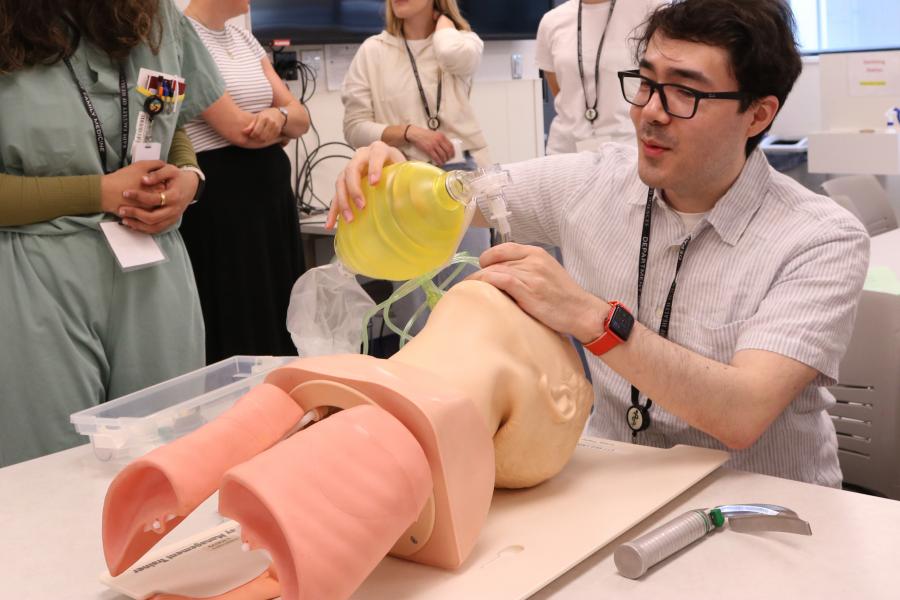
Simulation
Simulation applies simulation-based education (mannequins, scenario-based training, virtual reality, etc.) to teach and evaluate clinical skills, crisis management, teamwork and decision-making in safe environments. It also includes educational scholarship in simulation methodology.
Staff complement
- Dr. Cheryl ffrench serves as our simulation director
- Dr. Joey Ringaert serves as the simulation assistant director
Sports medicine
Sports Medicine focuses on the diagnosis, acute management, and rehabilitation of injuries and medical conditions occurring in athletes or physically active individuals. In the emergency setting, this often involves musculoskeletal injuries, concussion evaluation, and coordination with sports care networks.
Staff complement
- Dr. Deborah Hill serves as our Sports Medicine Fellowship director and works alongside Drs. Ali Almaleki and Eric Hildahl at the Pan Am Clinic.
Toxicology
Toxicology addresses the diagnosis, management, and prevention of poisoning, overdoses, and adverse effects of drugs or chemicals. This includes clinical consultation, antidote administration, and guiding protocols to improve patient safety and outcomes at the population level.
Staff complement
- Dr. Wesley Palatnick is one of the forebearers of emergency medicine in Manitoba and is internationally recognized for his work in the field of toxicology. He has contributed numerous articles, book chapters, lectures, and significant publications that have changed the way we all practice today.
- Dr. Palatnick serves as one of two clinical toxicologists providing on-call consultations for the entire province of Manitoba. Thousands of patients have benefited from his remarkable clinical expertise, compassionate care and tireless efforts.
Trauma
Trauma encompasses the management of patients who suffer significant injuries (e.g., from accidents, falls, violence). This includes rapid assessment, stabilization, coordinating multidisciplinary care, and working in regional trauma systems. Our emergency physicians often act as trauma team leaders and partners in trauma research.
Staff complement
Most emergency physicians working at the Health Sciences Centre serve as Trauma Team Leaders.
Dr. Julian Regehr serves as the trauma best practices lead.
Continuing education and professional development
Emergency Medicine Prairie Annual Conference (EMPAC)
This comprehensive full day conference covers up-to-date topics relevant to the emergency care of the undifferentiated patient, through lectures, workshops and skills sessions delivered by expert faculty from:
- emergency medicine;
- trauma;
- pediatrics;
- radiology; and
- wound care.
For questions or updates regarding the EMPAC 2026 conference, reach out to our continuing education and professional development program administrator at cepd.emergencymedicine@umanitoba.ca.
Advanced Cardiovascular Life Support (ACLS)
Advanced Cardiovascular Life Support (ACLS) is a video-based, Instructor-led, advanced course, that builds on the foundation of basic life support (BLS) skills.
It emphasizes the importance of continuous, high-quality CPR and takes healthcare provider training to the next level-highlighting the importance of high-performance team dynamics and communication, systems of care, recognition and intervention of cardiopulmonary arrest, immediate post-cardiac arrest, acute dysrhythmia, stroke, and acute coronary syndromes.
To learn more, reach out to our continuing education and professional development program administrator at cepd.emergencymedicine@umanitoba.ca.
SimAIRWAY: Foundations of Airway Management
SimAIRWAY: Foundations of Airway Management
This course is for physicians who want to learn, practice, and improve the skills and knowledge required for safe and effective airway management in an emergency setting. Skills include:
- bag-mask ventilation
- laryngoscopy and intubation
- airway adjuncts
- video laryngoscopy
- surgical airway
Principles of airway management covered include:
- approach to airway management
- airway pharmacology
- airway anatomy
- crisis resource management
SimA.R.T- Advanced Airway Management
This advanced course is designed for physicians seeking to refine and expand their expertise in emergency airway management. Developed by experienced emergency physicians, it integrates high-fidelity simulation with intensive hands-on practice to strengthen both technical proficiency and clinical decision-making.
| Date | Course | Register |
|---|---|---|
| January 19, 2026 | SimAIRWAY: Foundations of Emergency Airway Management | Register now |
| February 12, 2026 | SimAIRWAY: Foundations of Emergency Airway Management | Register now |
| March 2, 2026 | SimAIRWAY: Foundations of Emergency Airway Management | Register now |
| April 16, 2026 | SimAIRWAY: Foundations of Emergency Airway Management | Register now |
| May 7, 2026 | SimAIRWAY: Foundations of Emergency Airway Management | Register now |
To learn more about procedural sedation, reach out to our continuing education and professional development program administrator at
cepd.emergencymedicine@umanitoba.ca.
Procedural sedation
This simulation course offers a unique hands-on perspective on learning procedural sedation and analgesia, using a case-based format.
| Date | Course | Register |
|---|---|---|
| January 12, 2026 | Department of Emergency Medicine Procedural Sedation | Register now |
| January 29, 2026 | Department of Emergency Medicine Procedural Sedation | Register now |
| March 9, 2026 | Department of Emergency Medicine Procedural Sedation | Register now |
| March 25, 2026 | Department of Emergency Medicine Procedural Sedation | Register now |
| May 25, 2026 | Department of Emergency Medicine Procedural Sedation | Register now |
| June 12, 2026 | Department of Emergency Medicine Procedural Sedation | Register now |
To learn more about procedural sedation, reach out to our continuing education and professional development program administrator at
cepd.emergencymedicine@umanitoba.ca.
Simulation
CEPD courses that incorporate simulation and practical hands-on training are available throughout the academic year. These programs facilitate the effective application of crisis resource management skills in conjunction with real-time clinical decision-making.
Registration will open in the fall. Please watch for advertisements for the following courses, designed by emergency physicians for emergency physicians.
SimA.R.T. – SimTRAUMA
A three-hour course for physicians who want to learn, practice, and improve the skills and knowledge required for safe and effective management of the critically ill trauma patient.
SimA.R.T. – SimTOX
A three-hour course for physicians who want to learn, practice, and improve the skills and knowledge required for safe and effective management of the critically ill patient with a toxicologic emergency.
SimA.R.T. – SimPEDS
This three-hour course is for physicians who want to learn, practice, and improve the skills and knowledge required for safe and effective management of the critically ill infant and child in an emergency setting.
To learn more about procedural sedation, reach out to our continuing education and professional development program administrator at
cepd.emergencymedicine@umanitoba.ca.
Stay connected
If you would like to receive notifications when courses become available or have any questions regarding the program, please contact Kim Anderson, SIM education assistant by email: simulation.emergencymedicine@umanitoba.ca.
Ultrasound
With the growing demand for bedside ultrasound utilization for both postgraduate and undergraduate trainees, as well as for continuing professional development among staff physicians, the ultrasound section within the Department of Emergency Medicine (DEM) is an integral part of the academic curriculum for emergency residents and staff physicians.
These workshops have earned high praise from staff physicians for their organization, high instructor-to-learner ratio, and incorporation of pathology patients to simulate real-world clinical scenarios. The emergency medicine department at UM is recognized as a key leader in national POCUS education.
The CPD courses offered by the ultrasound section cover a wide range of topics, including:
- IP-core certification course
- IP-resuscitation certification course
- IP-diagnostic certification course
- IP-MSK certification course
- EGLS course
- Palliative/oncology course
- Soft tissue and foreign body workshop
- Peripheral and central line workshop
Staff complement
- Dr. Tomislav Jelic
| Date | Course | Register |
|---|---|---|
| January 28, 2026 | Ultrasound Guided Nerve Blocks | Register now |
| February 4, 2025 | Ultrasound Guided Nerve Blocks | Register now |
| February 13, 2026 | Intermediate Echo (CPD) | Registration opening soon |
| March 18-20, 2026 | IP Dx/MSK | Register now |
| May 14, 2026 | Echo/EGLS Course (full day) | Registration opening soon |
To learn more about ultrasound courses and registration, reach out to our ultrasound program administrator at ultrasound.emergencymedicine@umanitoba.ca.
Department Research
The Department of Emergency Medicine is committed to fostering and developing emergency medicine research locally, provincially and through both national and international collaborations.
Strengths
Directed by Dr. Murdoch Leeies, the Department of Emergency Medicine is developing particular strengths in the fields of COVID-19, health equity, pre-hospital emergency medicine, geriatric emergency medicine, ultrasound and critical care research. Our efforts have resulted in a multitude of peer-reviewed publications, poster presentations and funding awards.
Please consider a charitable donation to support innovative emergency medicine research at the University of Manitoba.
Achievements
Our achievements include:
- Our growing emergency medicine research program has produced over 100 publications in the last three years.
- A novel evidence-based medicine curriculum for EM trainees featuring enhanced critical appraisal and structured literature searching skills, quality improvement and implementation science modules as well as educational scholarship and knowledge translation content.
- A burgeoning department of collaborative clinician investigators working with national and international research networks, including CAEP and the Canadian COVID-19 Emergency Department Rapid Response Network.
Manitoba Emergency Medicine Research, Educational Scholarship & Quality Improvement Symposium
The annual Manitoba Emergency Medicine Research, Educational Scholarship & Quality Improvement Symposium (MB EM RESQI Symposium) is an opportunity to share and celebrate the scholarly work produced by staff, trainees and collaborators in the Department of Emergency Medicine.
Check back for information on the 2026 MB EM RESQI Symposium.
Community and partners
Manitoba Emergency Medicine Research Advancement Fund
In the emergency department, every second counts.
That’s why we’re working hard to stay at the leading edge of research that can help save lives and keep Manitobans healthy and active.
You can help.
In 2021, the Manitoba Emergency Medicine Research Advancement Fund was created to support the development of novel research in emergency medicine conceived of, designed by and conducted with Manitoban emergency medicine investigators.
Your generosity will directly support University of Manitoba Emergency Medicine students, educators and researchers to develop new work to better care for Manitobans in need of emergency medical care.

Events
Faculty and staff
Contact us
Emergency Medicine
S203 Medical Services Building
750 Bannatyne Avenue
University of Manitoba (Bannatyne campus)
Winnipeg, MB R3E 0W2 Canada